Introduction
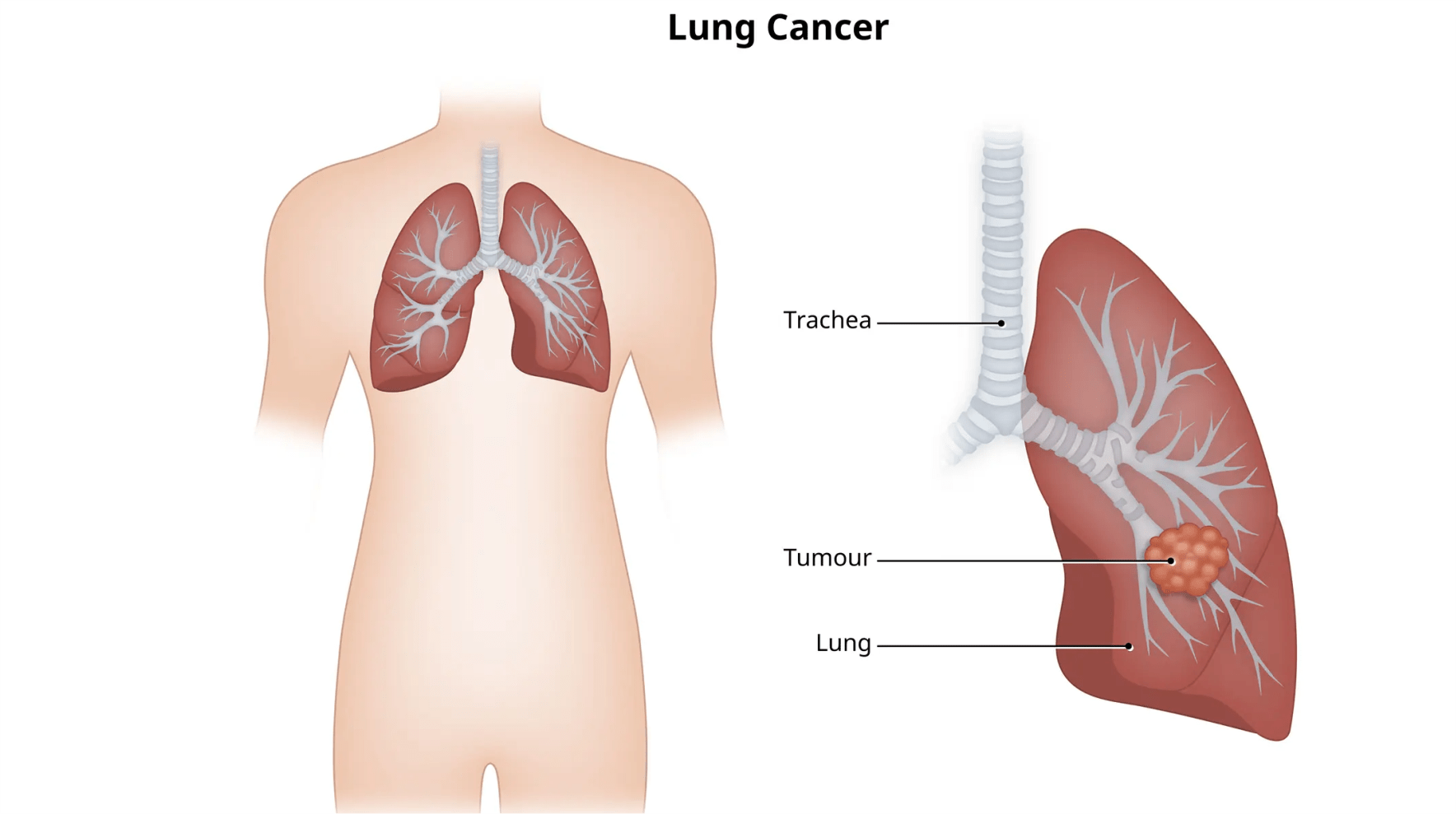
Lung cancer is often associated with smoking, but it’s crucial to recognize that non-smokers can also develop this deadly disease. Lung cancer in non-smokers is a growing concern worldwide, and its causes, risk factors, diagnosis, and treatment differ significantly from those associated with smoking-related lung cancer. In this comprehensive article, we will delve into the intricacies of lung cancer in non-smokers, shedding light on its prevalence, risk factors, molecular mechanisms, and promising research avenues. Hospitals like Punarjan Ayurvedic Cancer Hospital are famous for being one of the Best Cancer Hospital in Hyderabad.
The Prevalence of Lung Cancer in Non-Smokers
Lung cancer in non-smokers represents a substantial portion of all lung cancer cases. In some countries, such as the United States, it accounts for up to 15% of all lung cancer diagnoses. This percentage may seem relatively small, but when considering the global scale, it translates to a significant number of individuals affected by this disease. Understanding the prevalence of lung cancer in non-smokers underscores the urgency of studying its causes and developing effective prevention and treatment strategies.
Risk Factors
While smoking is the leading cause of lung cancer, non-smokers can develop the disease due to various risk factors:
Secondhand Smoke: Exposure to secondhand smoke, also known as passive smoking, is a significant risk factor for non-smokers. Inhalation of the carcinogens present in cigarette smoke increases the likelihood of developing lung cancer.
Radon Gas: Radon, a naturally occurring radioactive gas that can enter homes through the ground, is the second leading cause of lung cancer in non-smokers. Mitigating radon exposure through proper ventilation and testing is crucial.
Occupational Hazards: Certain professions expose individuals to carcinogens and toxins, such as asbestos and diesel exhaust, which can lead to lung cancer. Protective measures and workplace safety regulations are essential in reducing these risks.
Genetics: Genetic factors can predispose some non-smokers to lung cancer. Family history and specific genetic mutations, like EGFR and ALK, are associated with an increased risk of lung cancer in non-smokers.
Air Pollution: Exposure to high levels of air pollution, including fine particulate matter (PM2.5) and other environmental pollutants, can contribute to lung cancer development in non-smokers.
Molecular Mechanisms
Lung cancer in non-smokers often exhibits distinct molecular characteristics compared to smoking-related lung cancer. Two primary subtypes are prevalent among non-smokers:
Adenocarcinoma: Adenocarcinoma is the most common subtype in non-smokers. It tends to originate in the outer regions of the lungs and is frequently associated with genetic mutations, such as EGFR and ALK, making targeted therapies more effective.
Small Cell Lung Cancer (SCLC): While less common, SCLC is another subtype found in non-smokers. It is an aggressive form of lung cancer with fewer targeted treatment options available.
These distinct molecular profiles emphasize the need for personalized treatment approaches based on the specific genetic alterations present in each patient’s tumor.
Diagnosis and Screening
Diagnosing lung cancer in non-smokers can be challenging because it is often not considered a potential diagnosis in this population. Symptoms may overlap with other respiratory conditions, leading to delayed diagnosis. Therefore, early detection is crucial for improving outcomes.
Imaging: Chest X-rays and computed tomography (CT) scans are essential tools for identifying lung cancer. Low-dose CT screening is recommended for individuals at high risk, such as those with a family history, prior radiation exposure, or prolonged exposure to environmental toxins.
Biomarker Testing: Biomarker testing, including EGFR, ALK, and ROS1 mutations, can help identify specific treatment options for non-smokers with lung cancer.
Liquid Biopsies: Emerging technologies like liquid biopsies offer non-invasive ways to detect genetic alterations in lung cancer, enabling earlier diagnosis and treatment planning.
Treatment Options
Treatment for lung cancer in non-smokers depends on the stage and molecular characteristics of the tumor. Common treatment modalities include:
Surgery: Surgical resection is often the primary treatment for early-stage lung cancer in non-smokers.
Radiation Therapy: Radiation therapy may be used in conjunction with surgery or as a primary treatment for localized disease.
Targeted Therapies: Targeted therapies that address specific genetic mutations have shown remarkable success in treating non-smokers with lung cancer. Drugs like EGFR inhibitors and ALK inhibitors can significantly improve survival rates.
Immunotherapy: Immune checkpoint inhibitors have revolutionized the treatment of lung cancer, offering new hope for non-smokers with advanced disease.
Chemotherapy: Traditional chemotherapy remains a treatment option, particularly for advanced lung cancer cases.
Promising Research Avenues
The understanding of lung cancer in non-smokers has evolved rapidly in recent years, leading to promising research avenues:
Immunotherapy Advancements: Ongoing research is exploring combinations of immunotherapies, novel immune checkpoint inhibitors, and immunotherapy in early-stage lung cancer.
Liquid Biopsies: Continued development of liquid biopsy technologies may enable more precise and less invasive early detection and monitoring.
Genetic Research: Identifying additional genetic mutations and pathways involved in lung cancer in non-smokers can lead to the development of targeted therapies for previously untreatable cases.
Lifestyle and Prevention Studies: Research into the impact of lifestyle factors such as diet, exercise, and environmental exposure on lung cancer risk in non-smokers is essential for prevention strategies.
Conclusion
Lung cancer in non-smokers is a distinct entity with its own set of risk factors, molecular characteristics, and treatment approaches. Recognizing this subset of patients and understanding their unique needs is crucial for improving outcomes and reducing the global burden of lung cancer. Ongoing research and advancements in personalized medicine offer hope for better treatment options and increased survival rates for non-smokers diagnosed with lung cancer. Public awareness, early detection, and prevention efforts are key in the fight against this silent but deadly disease.